Contents
Fungal pneumonia (Pneumomycosis)
Fungal pneumonia – is a mycotic lesion of the lungs, the causative agents of which are various species of fungi. The disease is manifested by fever, weakness, cough with mucopurulent sputum and hemoptysis, shortness of breath, chest pain, myalgia. The diagnosis of fungal pneumonia is made on the basis of anamnesis, symptoms, lung radiography, microbiological, serological and molecular genetic studies. Treatment of fungal pneumonia includes prescription of antimycotic drugs, immunocorrectors, multivitamins, detoxifying and desensitizing agents.
ICD-10

General information
Fungal pneumonia (pneumomycosis) – an inflammatory process that develops in the alveoli and lung parenchyma with the introduction and uncontrolled reproduction of pathogenic or conditionally pathogenic strains of fungi. Fungal pneumonia can occur as an independent (primary) disease with direct infection of lung tissue or secondary, as a complication of another background disease, including a severe illness. ч. respiratory pathology (bronchiectatic disease, obstructive bronchitis, lung abscess).
Fungal pneumonia is considered one of the most severe forms of pneumonia, the number of cases of which has recently increased, despite the use of the latest antimycotic drugs in pulmonology. Specificity of causative agents and a torpid course of pneumomycoses are very difficult for an accurate diagnosis and delay timely treatment, exacerbating inflammatory changes.

Causes
The cause of fungal pneumonia is colonization of the mucosa of the lower parts of the respiratory tract with strains of fungi, many of which are representatives of the opportunistic microflora. The causative agents of the disease can be fungi of different species – molds (Aspergillus, Mucor), yeasts (Candida), endemic dimorphs (Blastomyces, Coccidioides, Histoplasma), pneumocysts (Pneumocystis). The most common fungal pneumonia is caused by Candida fungi (C. albicans), aspergillus and pneumocysts (P. carinii), which have preferential tropism to lung tissue.
Depending on the causative agent, pneumomycoses are divided into:
Pathogenic fungi, the causative agents of exogenous pneumomycoses (Aspergillus, Mucor, Blastomyces, Coccidioides, Histoplasma) may be present in soil, water, industrial and household dust, in damp rooms, on rotten wood, untreated medical equipment and enter human lungs mainly by inhaling air contaminated with mycelium and spores (air-drop-dust route). The causative agent of pneumocystis pneumonia is transmitted only from person to person. First, a temporary and then a persistent carrier is formed with the development of fungal pneumonia.
Fungal pneumonia can manifest as mixed infection (mixed, caused by different types of fungi – yeast-like and mold-like) and combined, caused by fungi and other microorganisms (e.g., aspergillus with gramnegative microflora). Thoracic actinomycosis is a pseudomycosis, because it is caused by anaerobic bacteria of the genus Actinomyces and is accompanied by the formation of an infectious granuloma (actinomycoma) with protrusion into the surrounding tissue and formation of purulent fistulas.
The causative agents of endogenous fungal pneumonia enter the lungs from other foci of mycosis in the body: by aspiration (for example, in candidiasis of the mouth cavity, trachea, bronchi) or hematogenous and lymphogenous – in case of widespread lesion. Candida fungi present in the microbiocenosis of the skin and mucosa of the respiratory tract under certain conditions become active, acquire pathogenicity and cause pneumomycosis.
Risk factors
Fungal pneumonia often develops in patients with malignant blood diseases (acute leukemia) and lymphoproliferative tumors receiving long-term radiation or systemic chemotherapy (immunosuppressants and glucocorticoids); as a complication of HIV infection and AIDS, diabetes, aplastic anemia, tuberculosis, conditions after organ transplantation, artificial ventilation. The occurrence of fungal pneumonia is contributed by the violation of normal microflora (respiratory dysbacteriosis), associated with prolonged and irrational use of antibiotics. Among the main factors of development and reactivation of fungal pneumonia in 50% of patients is agranulocytosis. Fungal pneumonia is often combined with mycotic lesions of mucous membranes, skin, nails.
Pathogenesis
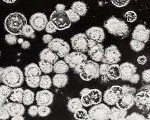
The realization of the pathogenic potential of fungi always contributes to the suppression of specific and non-specific general and local resistance factors of the body with the development of immunodeficiency state. Inoculating lumen of bronchioles and alveoli the fungi begin to multiply actively, causing migration of leukocytes and accumulation of serous fluid. In the period of exacerbation mycotic lesions of lung tissue are characterized by the presence of decay zones in the form of cavities, sometimes – by the formation of abscesses, in which accumulations of fungus are found; in the period of recovery, areas of dense granulation tissue appear in their place.
Symptoms of fungal pneumonia
In most cases, the onset of pneumomycosis is characterized by a vague clinical picture, with minor, sometimes atypical symptoms and manifested by episodes of fever, weakness, dry cough, myalgia. Intoxication associated with the action of mycotoxins. The appearance of purulent sputum at the rupture of abscesses formed by the accumulation of fungi in the lung tissue, makes the picture of the disease more pronounced.
Massive single infection with exogenous fungi provokes an acute process, in case of repeated inflow of small doses of pathogens and in weakened patients pneumomycosis takes a chronic course with relapses. Excessive development of connective tissue leads to shortness of breath, streaks of blood in the sputum (sometimes, profuse pulmonary bleeding). Mixed forms of pneumomycoses are more severe than monoinfections. Fungal pneumonia can be complicated by exudative or fibrinous pleurisy when the abscess is opened into the pleural cavity or when the fungus invades the pleura; by the development of respiratory (including pulmonary) disease. ч., acute) and cardiovascular failure. The course of pneumomycoses of various etiologies has certain clinical features.
Aspergillosis of the lungs
Aspergillosis pneumonias may be acute or chronic, including severe lightning-type forms. They are often characterized by signs of abscessed pneumonia, possible involvement of the pleura and lymph nodes, as well as the formation of specific pustular granulomas. Almost constant attacks of cough with profuse mucopurulent or purulent discharge (in the form of tight lumps) and an admixture of blood, pain and heaviness in the chest, shortness of breath turning into suffocation, prolonged subfebrile symptoms with temperature jumps, chills and night sweats. Severe general condition, severe weakness, anorexia and cachexia are observed.
Infiltration of vascular walls with the formation of thrombosis and hemorrhagic infarcts by fungi is possible. Chronic aspergillus pneumonia is secondarily superimposed on various lung lesions, manifesting as symptoms of the underlying disease and fungal affection. Localized form – pulmonary aspergilloma occurs when fungi infect an already existing cavity in lung tissue and is often asymptomatic. In fungal pneumonia, abscessing may become a chronic process.
Lung candidiasis
Primary candidiasis pneumonia may be accompanied by signs of intoxication with normal body temperature, sometimes it may begin acutely with fever, shortness of breath, cough with poor sputum, hoarseness of voice, chest pain, increased sweating. Bilateral lesions are typical, and in young children a relapsing course is possible with progression to chronic granulomatous generalized candidiasis. Secondary candidiasis pneumonia is severe with a strangling cough, purulent bloody sputum, vomiting, dehydration. Often it becomes a progressive destructive process with formation of large thin-walled cysts in the lungs, development of pulmonary atelectasis, miliary dissemination or septic condition.
Pneumocystis pneumonia
Pneumocystis pneumonia occurs as a mono- or mixt-infection, often asymptomatically or with a vague clinical picture, and may be latent in the first years of life. The possibility of subsequent reinfection is not uncommon. It is characterized by the gradual increase of hypoxemia and respiratory disorders, prolonged unproductive cough against the background of poor physical and radiographic data. Premature infants have a manifest form of pneumocystis pneumonia with prolonged, severe respiratory failure. Appearing the first of the opportunistic infections in immunocompromised patients, pneumocystis has a rather long period of lethargy, complicated by spontaneous pneumothorax, accession of superinfection. Fatal outcome without specific treatment.
Diagnosis
Determination of the genesis of fungal pneumonia is often difficult due to the peculiarity of mycotic infection, so a comprehensive approach with the analysis of anamnesis, clinical symptoms, results of lung X-ray, microscopic, cultural, serological (ELISA, RAS, PHA, RNIF) and molecular-genetic (PCR) studies of sputum, blood, lavage and pleural fluid, pulmonary tissue aspirates.
Aspergillosis reveals a picture of abscessed pneumonia and the phenomenon of purulent bronchitis. If there is evidence of previous antibiotic treatment and no response to therapy, fungal pneumonia may be initially suspected. The presence of a focus of mycosis in the form of oral thrush gives reason to think about the candidal nature of the disease. It should be taken into account that in the presence of an immunodeficiency state, the risk of developing fungal pneumonia is much higher.
With fungal pneumonia, a general practitioner or pulmonologist will auscultate in the lungs multiple, first dry, then wet multi-caliber rales. The patient’s blood reveals eosinophilic leukocytosis with a shift to the left and increased sedimentation. X-rays show an intensification of the pulmonary pattern, infiltrative shadows of small or huge size with uneven edges; if abscesses appear, chaotically arranged cavities with fluid levels are seen.
In pneumomycosis, fungal spores and mycelium can be detected by microscopy of sputum smear and bronchoalveolar fluid. Sputum bacterial examination is important prior to treatment, which increases the likelihood of isolation and identification of the causative agent of fungal pneumonia and its quantification. Direct detection of DNA and identification of the strain of fungus in sputum by PCR should be correlated with the presence of clinical manifestations of the disease. The mere fact of fungal colonization of the respiratory tract in the absence of symptoms of infectious lesions is not sufficient for a diagnosis of fungal pneumonia. PCR blood tests for fungi can differentiate between disseminated and local forms of mycosis.
Material from the distal bronchi is obtained by bronchoscopy with bronchoalveolar lavage. In the flush, the causative agent of pneumocystis pneumonia is detected in 89–98% of cases. If necessary, aspirate (biopsy) by puncture or open lung biopsy is indicated. PCR in case of fungal pneumonia is informative even after the beginning of antibiotic therapy and allows simultaneous detection of DNA of different pathogens in case of co-infection. At serodiagnostics the analysis of dynamics of detection of antibodies to potential causative agents of fungal pneumonia is indicative.
Treatment of fungal pneumonia
As in case of fungal pneumonia the use of antibiotics will lead to aggravation of the course of the disease, the prescription or specific antimycotic drugs (itraconazole, amphotericin B, fluconazole, ketoconazole, etc.) is required.), or folic acid inhibitors and clindamycin in pneumocystis.
In fungal pneumonia, immunocorrective drugs, multivitamins, detoxifying and stimulating agents, a rational regime and diet are used to eliminate immune deficiency. In the case of fungal-bacterial pneumonia, a short course of antibiotics is indicated, and if combined with allergic symptoms, desensitizing drugs and corticosteroids are used. When pneumomycosis is complicated by exudative pleurisy, pleural puncture and pleural cavity lavage are performed.
Prognosis and Prevention
Accurate prompt diagnosis and therapy make the prognosis of fungal pneumonia encouraging. Risk of severe complications if treatment is untimely and inadequate. Fungal pneumonia is one of the most common causes of death in patients with AIDS. With a favorable prognosis of primary aspergillosis and candidiasis, the tendency for inflammatory respiratory tract disease and fungal sensitization may persist; and pulmonary complications (pneumosclerosis) may lead to disability of the patient. In secondary fungal pneumonia, prognosis depends on the severity of the underlying background disease.
Prevention of fungal pneumonia includes prophylaxis in production and agriculture (sealing of technological processes associated with dust production, the use of respirators, microbiological control of the environment), in medicine and the food industry (compliance with disinfection and sterilization). Individual prevention involves strengthening the immune system, eliminating dysbacteriosis and chronic pathology, carrying out rational antibiotic therapy.