Contents
Esophageal candidiasis (Candida esophagitis)

Esophageal candidiasis — It is a mycotic infection that is caused by fungi of the genus Candida. The disease is manifested by difficulty in swallowing, retrosternal pain, and discomfort. If candidiasis persists for a long time, weight loss, severe avitaminosis. The basis for the diagnosis of fungal infection is an examination of the esophagus during EFGDS with subsequent morphological analysis of biopsy specimens to detect particles of the pathogen. In addition, microbiological culture of biomaterial is performed. For treatment of esophageal candidiasis, antifungal drugs of different chemical structure of systemic action are used.
ICD-10
General information
Esophageal candidiasis (candidiasis esophagitis) is considered an opportunistic infection. The incidence of the disease among general patients is 1-2%, with the presence of diabetes mellitus occurs much more frequently — In 5-10% of cases. In patients with HIV infection and AIDS, the prevalence of esophageal fungal infections reaches 30%. Incidence of candidiasis among the elderly is 2 times higher than the average in the population, in old age (after 75 years) — 6 times higher. Infection sometimes occurs in children against a background of primary immunodeficiencies.
Causes
The causative agents of this infectious esophageal disease are fungi of the genus Candida. There are more than 150 species of Candida fungi in total, but in 60-90% of cases the pathology is caused by C. albicans. In immunosuppression, the role of other species increases — C. Drug immunosuppression, C. kefir, C. lucitanies and C. krusei. Microorganisms are naturally occurring in the form of blastomycetes or pseudomycelia. A number of predisposing factors contribute to the development of candidiasis:
- Immunodeficiencies. Damage of digestive tract mucosa by Candida fungi is one of the markers of progressive HIV infection. High incidence of the disease is observed in primary genetically conditioned immunodeficiencies: DiGeorge syndrome, Bruton syndrome, Wiskott-Aldrich disease, etc.
- Drug immunosuppression. The incidence of candidiasis increases with prolonged treatment with corticosteroids, which depress the activity of the immune system. Radiation and chemotherapy of cancer patients has a negative impact, which disrupts local and general immune defense factors.
- Endocrine diseases. The probability of occurrence of mycosis increases in patients with diabetes mellitus, autoimmune polyendocrine syndrome, hypothyroidism. Antifungal resistance is reduced in obesity and other manifestations of metabolic syndrome.
- Local factors. Local causes of mycotic process include chronic inflammatory and atrophic changes in the esophageal wall, xerostomia, degenerative and destructive disorders in the oral cavity. The pathology is twice as common in those who use removable dentures.
Risk factors
Risk factors for esophageal candidiasis: emaciation, avitaminosis, chronic somatic diseases accompanied by asthenia. The likelihood of mycosis increases after organ transplant surgery.
Prevalence of candidiasis in the aged is connected with the involutionary waning of immunity functions, microcirculation disorders due to atherosclerosis, atrophy of esophageal mucous layer. Polypragmasy, in particular uncontrolled use of antibiotics, hormones and antisecretory drugs, plays a great role in the formation of candidiasis.
Pathogenesis
The first step in the mechanism of disease development is adhesion (attachment) of fungal cells to the surface of the esophageal mucosa. Subsequently, the microorganisms are able to transform into filamentous form and invade deeper layers of the esophageal wall. Tissue damage results from production of specific enzymes by the pathogen. Defects in T-cell immunity play a major role in the candidiasis manifestation.
The nature of the infection is determined by the state of antifungal protection factors of the body. When the immune system works properly, transient transmission occurs. With defects in the immune system, a persistent carrier without clinical symptoms usually occurs. If one or more of the conditions are present, the typical candidiasis develops.
Classification
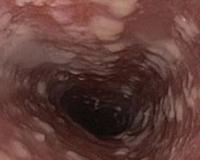
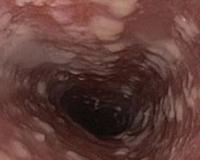
According to the anatomical classification, the lesion of the esophagus by candida fungi belongs to the superficial forms of candidiasis. In practical gastroenterology, endoscopic classification is widely used, which is necessary to systematize the different variants of lesions of the esophageal mucosa. Clinicians distinguish 3 variants of changes in the esophagus in candidiasis:
- Catarrhal esophagitis. Characterized by hyperemia of esophageal mucosa and moderate edema. Candida infection is indicated by a thin, spider-like plaque on the epithelium, contact bleeding.
- Fibrinous esophagitis. In the esophagus, whitish-gray plaques up to 0.5 cm in size form. Hyperemia, swelling and bleeding of the mucosa are more intense than in the catarrhal form.
- Fibrinous erosive esophagitis. Candidiasis is manifested by multiple plaques of a dirty gray color, after removal of which erosions are visualized on the mucosa. Spontaneous bleeding is characteristic.
Esophageal candidiasis symptoms
Typical signs of esophageal candidiasis — Difficulty and pain at the time of swallowing. The person feels discomfort when eating solid and dry food, but does not feel uncomfortable when drinking. Painful sensation as food lumps pass down the esophagus. Some patients wash down each bite of food with water to relieve pain and burning.
Sudden discomfort in the chest, which occurs regardless of the consumption of food. Less frequent occurrence of unpleasant-smelling belching, heartburn. If the esophagus is severely affected, it hurts a lot when eating, so patients reduce the number and amount of meals. Weight loss due to prolonged malnutrition and the accompanying symptoms of avitaminosis.
Complications
Most common consequence of undiagnosed candidiasis — Stricture formation in the upper half of the esophagus — Occurs in 8-9% of cases. Scar deformity of the organ is accompanied by permanent dysphagia of both solid and liquid food, requiring surgical correction. Dissemination of mycotic infection with development of deep candidiasis of internal organs and sepsis is considered a dangerous complication.
Owing to the contact vulnerability of mucosa, constant, low-intensity bleeding is typical if pieces of poorly chewed food injure the esophagus. Chronic bleeding leads to iron deficiency anemia. In patients suffering from thrombocytopenia, profuse bleeding with hemorrhagic shock is possible. Very dangerous esophageal perforation, which manifests as painful shock, pneumomediastinum, and subcutaneous emphysema of the neck.
Diagnosis
With esophageal candidiasis, there are no pathognomonic symptoms, so the diagnostic search includes a number of laboratory and instrumental methods. Sometimes during examination, the gastroenterologist notices foci of fungal lesions of the oral cavity, which indirectly indicates a mycotic etiology of dysphagia. The following examination methods are used to confirm the diagnosis:
- Esophagogastroduodenoscopy. During endoscopic examination of the mucosa, typical changes are visualized, which are described in detail in the classification. During EFGDS, a biopsy of the area with suspicious plaque is taken. To exclude concomitant gastrointestinal diseases, the stomach and the initial sections of the 12 duodenum are necessarily examined.
- Biopsy examination. Cytological and histological analysis of biomaterial of esophageal mucosa — «gold standard» esophageal candidiasis diagnosis. After special staining under a microscope, blastomycetes are detected, which indicates the presence of Candida fungi, or pseudomycelium — Sign of active infection.
- Cultural method. A culture of the plaque from the esophagus on nutrient media is performed to detect the species identity of the pathogenic fungus. Then the sensitivity test of the pathogen to the main antimycotic drugs is carried out, which is necessary for the rational choice of the treatment regimen.
Treatment of esophageal candidiasis
Candida infections are treated with specific antifungals. They inhibit the synthesis of the chemicals that make up the cell wall of the fungus. There are 3 groups of antimycotics, which differ in the degree of absorption when taken orally. Azole antifungal drugs are most frequently used in clinical practice, and they have to be taken for 2-3 weeks.
If the standard regimen is not effective, the antimycotic is changed or the drug is given parenterally. Treatment with the drug lasts until clinical and laboratory symptoms have completely disappeared. For AIDS patients, an obligatory condition for cure is decreasing viral load and increasing CD4-cells level. Modern antiretroviral therapy regimens are recommended for this.
Prognosis and prevention
The likelihood of complete recovery depends on the conditions and causes of the candidiasis. In people with normal immune status, the prognosis is favorable — Cure requires 1 course of antifungal therapy. If a patient is HIV-infected, or if he or she is taking immunosuppressive medications, there is a risk of recurrent fungal infection.
Primary prevention measures include controlled administration of immunosuppressants and antibiotics, early detection and treatment of oropharyngeal candidiasis. To prevent relapses, immunocompromised patients are indicated to take a daily antifungal drug at a low dose. Less commonly, prophylactic weekly doses of doubled doses of an antimycotic are used.